Pregnancy and
diabetes
Planning pregnancy, lowering the risks, and contraception
Planning a healthy pregnancy when you live with type 2 diabetes will help lower the risk of complications to you and your baby.
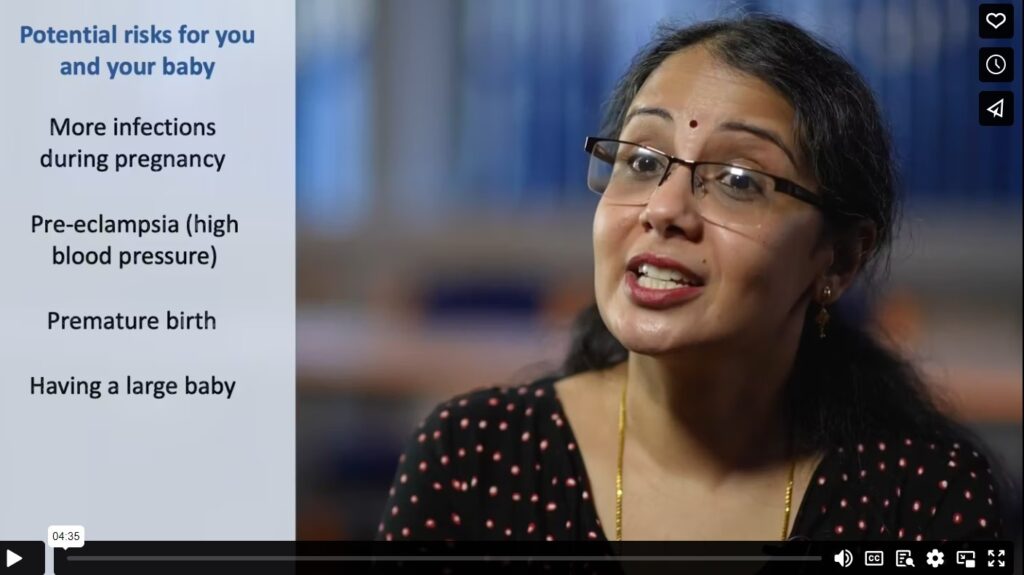
What are the risks to you?
- Having a miscarriage
- Problems with eyes and kidneys
- Having a larger baby which can cause problems during labour.
- Developing pre-eclampsia
What are the risks to your baby?
- Heart problems, spina bifida and other disabilities.
- Being stillborn or dying shortly after birth.
- Problems after birth that require special or intensive hospital care.
Letting your GP or diabetes team know before you start trying for a baby gives you time to get your body ready for a healthy pregnancy.
We have created a ‘Baby Ready Checklist’ for you to follow:
Baby Ready Checklist
-
Agree a plan with your healthcare team – organise this at least 12 weeks before trying to get pregnant. This will ensure all your medications, blood tests, and eye screenings are up to date.
-
Start taking 5mg Folic Acid daily – This can only be prescribed by your GP and helps prevent neural tube defects (spina bifida). Take 5mg Folic Acid for at least 3 months before pregnancy, and for the first 12 weeks after you become pregnant.
-
Take Vitamin D daily – Between 800-1000 IU is recommended, both before and during your pregnancy.
-
Maintain a healthy body weight and stay active – This improves your chances of getting pregnant, helps your glucose control, and overall health during pregnancy.
-
Review any current medications with your Diabetes clinician – Current medications should be reviewed before getting pregnant. Avoid suddenly stopping medications unless specifically advised by your GP or diabetes Nurse. They will also tell you which medicines are safe to take in pregnancy.
- Closely and regularly monitor your blood glucose levels – If you aren’t already doing this you will be asked to do so by your GP or Diabetes Nurse as it is important. We will offer you additional support to achieve the ideal target ranges below:
- Finger prick tests: Ideal home glucose monitoring levels (finger-prick tests) are less than 5.3mmol/l before meals, and below 7.8mmols/l 1 hour after meals.
- Continuous Glucose Meter: The ideal range for pregnancy is 3.9-7.8 mmol/l and you should aim for a Time in Range (TIR) of 70% or more.
Contraception
In general, women with diabetes can choose from the same types of contraception as anyone else. If you have other medical conditions, discuss options with your healthcare team. When living with diabetes there are increased risks during pregnancy to you and your baby, so it’s important to plan ahead.
What if I get pregnant without planning it?
Don’t Panic! And don’t immediately stop your medications – it could be more harmful if your blood glucose or blood pressure suddenly become high in the first weeks of pregnancy. Speak to your practice nurse or a diabetes midwife on the numbers below and they will make a plan to adjust the medications quickly and safely.
As soon as your pregnancy is confirmed by an at-home pregnancy test, contact the Diabetes Specialist Midwife via the relevant area details below for an appointment.
Diabetes Specialist Midwife contact details:
Buckinghamshire: 01296255790 or bht.maternitydiabetesmidwifery@nhs.net
Oxfordshire: 01865 851039 or Diabetes.Midwives@oxnet.nhs.uk
Berkshire West: 0118 322 7245 or rbft.diabetes-midwife@nhs.net